Healthcare organizations and associations put pressure on Congress to help bolster home care models
March 2022 – The Journal of Healthcare Contracting
By Daniel Beaird
A recent report from McKinsey & Co. stated that as much as $265 billion worth of care services for Medicare fee-for-service and Medicare Advantage beneficiaries could shift to the home by 2025, representing a three- to fourfold increase in the cost of care being delivered at home for this population.1 The COVID-19 pandemic accelerated this movement and a significant portion of it came through Hospital-at-Home (HAH) programs, which enable some patients who need acute-level care to receive it in their homes rather than in a hospital, thus aiming to reduce costs, improve outcomes and enhance the patient experience.

CMS launched the Acute Hospital Care At Home program in November 2020, during the first year of the pandemic. It provided hospitals the flexibility to care for patients in their homes, originally helping relieve facilities of non-COVID patients to assist in tackling the surge of COVID-positive patients. As many HAH programs evolved throughout the pandemic, they shifted to enrolling COVID-positive patients as well to finish their hospitalization at home. Now, COVID-positive are enrolled directly from emergency departments.
“One driver to more enrollments is the barrier of obtaining reimbursements for short-term oxygen,” Peter Read, MD, medical director of Des Moines, Iowa-based UnityPoint Health’s hospital-at-home program, told AHA’s Advancing Health podcast in February.2 “We worked with our ACO to develop a waiver that allows us to dispense short-term oxygen to overcome reimbursement.” UnityPoint Health has achieved $900,000 in shared savings from just its hospital-at-home program, and many of its other home-based services were in increased demand due to the pandemic. The Midwestern health system has enrolled over 150 patients in its program and averted over 100 hospitalizations during the pandemic.
Advanced Care at Home Coalition
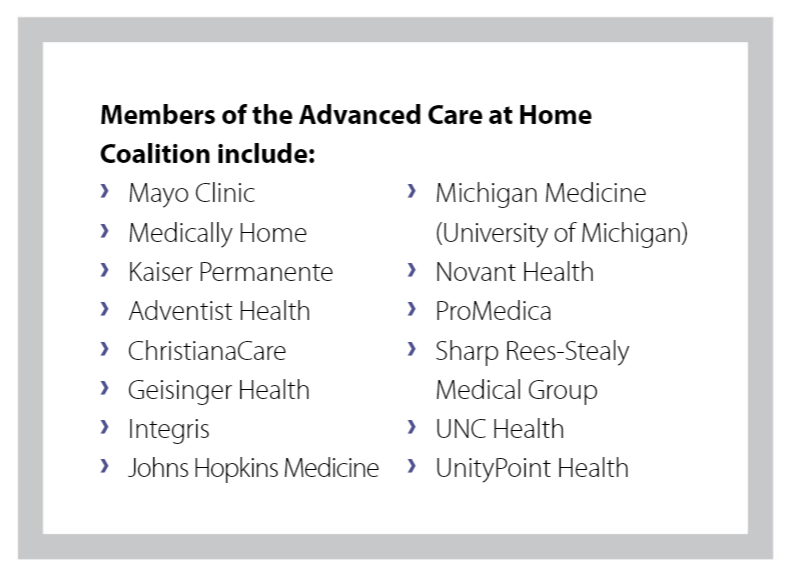
UnityPoint Health is part of the Advanced Care at Home Coalition led by a steering committee comprised of the three founding members, including Mayo Clinic, Kaiser Permanente and Medically Home. Its 12 other members is a list of prominent health systems, including Baltimore-based Johns Hopkins Medicine, which was a leader under Bruce Leff, MD, in these programs in the mid-1990s. The coalition has applauded the recent introduction of the Hospital Inpatient Services Modernization Act, which would extend the Acute Care at Home waivers that have allowed expanded delivery of hospital-level care at home for Medicare beneficiaries during the pandemic.
The bipartisan legislation sponsored by Sens. Tom Carper (D-DE) and Tim Scott (R-SC), and Reps. Brad Wenstrup (R-OH) and Earl Blumenauer (D-OR) extends the waivers for two years beyond the duration of the COVID-19 public health emergency and it requires CMS to issue regulations establishing health and safety requirements for Acute Hospital Care at Home programs within one year of the bill’s enactment. It’s supported by more than 100 health organizations and healthcare associations.
“By extending these flexibilities, Congress will create a predictable pathway for medical professionals to fully realize advances in the care delivery system that enable patients to be treated with safe, equitable, person-centered care in the comfort of their own homes,” said Stephen Parodi, MD, executive vice president of The Permanente Federation at Kaiser Permanente, which has provided hospital-level care at home to more than 1,100 patients.
“We adapted to COVID-19 by developing pathways to deliver the COVID-19 vaccine to those unable to obtain one through traditional pathways,” added Dr. Read. “We are also testing patients for COVID-19 who are unable to leave their homes. In the future, we would like to begin administering monoclonal antibody treatment at home for those COVID-positive patients at high risk for complications.”
Mount Sinai’s model
New York-based Mount Sinai Health System was awarded a Center for Medicare and Medicaid Innovation (CMMI) award in 2014 to launch its hospitalization-at-home program, building upon its home-based primary care program for homebound patients in Manhattan, N.Y.
“I had always been frustrated as a primary care physician in someone’s home where I knew the patient had pneumonia and needed an IV and antibiotic, but because of all the rules, regulations and prior authorizations, I couldn’t treat them with IV antibiotics at home very easily,” said Linda DeCherrie, MD, clinical director of Mount Sinai at Home, to the AHA.3
When Mount Sinai received the project grant from CMMI, the patients they took care of were Medicare fee-for-service patients for three years of the grant. After that, it had to pivot to Medicare Advantage plans, commercial and managed Medicaid. It formed a joint venture with Nashville, Tenn.-based Contessa Health in 2017 for the ability to negotiate with various insurance plans for bundle payments. Contessa Health aids its provider partners in addressing these challenges in the new standard of care.
Negotiation challenges are some of the biggest barriers for these programs starting up around the country, according to Dr. DeCherrie, but Mount Sinai’s program has been very successful and popular with patients.
“I don’t think we had a single patient decline joining the program,” said Dr. DeCherrie. “People were wanting to get out of the hospital, especially during the height of the pandemic with a no visitor policy. They wanted to go home as soon as they could.”
The New York health system launched the second part of its program during the pandemic and called it Completing Hospitalization-at-Home. This was aimed at patients who had been in the hospital, even as a COVID-positive patient in the ICU but were on a healing trajectory.
Some of the state of emergency waivers allowed Mount Sinai to implement the program. They had it up and running within two weeks of the issued state of emergency. It began with non-COVID patients, but eventually extended to COVID-positive patients.
Future of home care
The pandemic has accelerated the adoption of home care, and the emergence of new technologies has helped its acceptance. The Mayo Clinic found remote patient monitoring effective for ambulatory management of patients with a 78.9% engagement rate during the pandemic, and 11.4% and 9.4% 30-day emergency department visit and hospitalization rates, according to McKinsey & Co.
A patient with coronary artery disease, for example, can be evaluated by a physician and sent home, assigned a nurse and care manager, remote patient monitoring and have meals delivered to their home by community-based organizations.
For UnityPoint Health in Iowa, it expects each full-time equivalent physician and nurse practitioner in its hospital-at-home program to produce six units of service per day, measured by an 80-minute block of time that includes all drive time, documentation, visit and care coordination. Dr. Read explained that two units of service per day is dedicated to a new patient and one unit of service per day to a follow-up patient. The goal is to mix and match new patients with follow-up patients resulting in four patient encounters per day. An on-call provider is also available 24/7.
“We round on our active patients seven days per week,” said Dr. Read.
1 From facility to home: How healthcare could shift by 2025
2 Hospitals at Home with UnityPoint Health
3 Members in Action: Mount Sinai Health System
