Primary Cares Initiative is a further step in physician payment reform
 Primary care physicians are cautiously optimistic about a new primary-care payment program unveiled in April by the Centers for Medicare & Medicaid Services. The new model – Primary Cares Initiative – is intended to build on CMS’ prior programs to reimburse primary care physicians on the basis of health and outcomes rather than on a per-procedure basis.
Primary care physicians are cautiously optimistic about a new primary-care payment program unveiled in April by the Centers for Medicare & Medicaid Services. The new model – Primary Cares Initiative – is intended to build on CMS’ prior programs to reimburse primary care physicians on the basis of health and outcomes rather than on a per-procedure basis.
“APC members have expressed a lot of interest and desire to participate in these types of innovative new payment models that reward clinicians for keeping patients healthy,” says Robert McLean, M.D., FACP, president of the American College of Physicians, a specialty organization for internal medicine physicians. “Up until now, one of the main criticisms we’ve heard and one that we’ve repeatedly relayed to CMS is that we need more [alternative payment models]. So, at a high level, we’re certainly excited to see the CMS Innovation Center start to come out with new models, and hope that is just the tip of the iceberg and we have more coming.”
The CMS Primary Cares Initiative will provide primary care practices with five new payment model options under two paths: Primary Care First (PCF) and Direct Contracting (DC). The five options are:
- Primary Care First (PCF)
- Primary Care First – High Need Populations
- Direct Contracting – Global
- Direct Contracting – Professional
- Direct Contracting – Geographic
Primary Care First
The Primary Care First model will be tested for five years and is scheduled to begin in January 2020. (A second application round is planned for participants starting in January 2021.) Eligible practitioners are those in internal medicine, general medicine, geriatric medicine, family medicine, and/or hospice and palliative medicine. CMS says it will encourage other payers – including Medicare Advantage Plans, commercial health insurers, Medicaid managed care plans, and State Medicaid agencies – to align payment, quality measurement, and data sharing with CMS in support of Primary Care First practices.
Both paths under PCF are intended to incentivize providers to reduce hospital utilization and total cost of care by potentially rewarding them through performance-based payment adjustments, says CMS. These models seek to improve quality of care, specifically patients’ experiences of care and key outcomes-based clinical quality measures, which may include controlling high blood pressure, managing diabetes mellitus, and screening for colorectal cancer.
PCF payment model options “will test whether financial risk and performance-based payments that reward primary care practitioners and other clinicians for easily understood, actionable outcomes will reduce total Medicare expenditures, preserve or enhance quality of care, and improve patient health outcomes,” said CMS in a statement. PCF will provide payment to practices through a total monthly payment. It will also include a payment model option that provides higher payments to practices that specialize in care for high-need patients, including those with complex, chronic needs and seriously ill populations.
Direct Contracting option
While the two PCF models are focused on individual primary care practice sites, the three Direct Contracting payment model options aim to engage organizations that have experience taking on financial risk and serving larger patient populations, such as accountable care organizations, Medicare Advantage plans, and Medicaid managed care organizations, according to CMS.
The DC options are designed to financially reward organizations that offer greater efficiencies and better quality of care, the agency says. The options include a focus on care for patients with complex, chronic needs and seriously ill populations, as well as a voluntary option that allows beneficiaries to align with the healthcare provider of their choosing.
Depending on the DC payment option in which an organization is participating, the model participant will receive a fixed monthly payment that can range from a portion of anticipated primary care costs to the total cost of care. Participants in the global payment model option will ultimately bear full financial risk, while those in the professional payment model option will share risk with CMS.
CMS anticipates these five payment model options administered under the Primary Cares Initiative will:
- Provide better alignment for over 25 percent of all Medicare fee-for-service beneficiaries. More than 11 million Medicare beneficiaries would potentially be included (5 million beneficiaries in the DC payment model options and 6.4 million in PCF payment model options).
- Offer new participation and payment options for an estimated one in four primary care practitioners as well as other healthcare providers.
- Create new coordinated care opportunities for a large portion of the 11-12 million beneficiaries dually eligible for Medicare and Medicaid, specifically those in Medicaid managed care and Medicare fee-for-service.
Builds on CPC+
Primary Care First borrows underlying principles from the Comprehensive Primary Care Plus (CPC+) model, which was introduced in January 2017, says CMS:
- Prioritizing the doctor-patient relationship
- Enhancing care for patients with complex chronic needs and high need, seriously ill patients
- Reducing administrative burden
- Focusing financial rewards on improved health outcomes
More than 2,900 primary care practices and 56 aligned payers participate in CPC+ in 18 regions: Arkansas, Colorado, Hawaii, Greater Kansas City Region of Kansas and Missouri, Louisiana, Michigan, Montana, Nebraska, North Dakota, Greater Buffalo Region of New York, North Hudson-Capital Region of New York, New Jersey, Ohio and Northern Kentucky Region, Oklahoma, Oregon, Greater Philadelphia Region of Pennsylvania, Rhode Island, and Tennessee.
What’s next?
“For years, policymakers have talked about building an American healthcare system that focuses on primary care, pays for value, and places the patient at the center,” said Health and Human Services Secretary Alex Azar, when the Primary Cares Initiative was unveiled in April. “These new models represent the biggest step ever taken toward that vision.
“Building on the experience of previous models and ideas of past administrations, these models will test out paying for health and outcomes rather than procedures on a much larger scale than ever before.”
CMS is seeking public comment on one DC payment model – the Geographic Population-Based option – with an expected launch in January 2021. The option is designed to offer organizations the opportunity to assume responsibility for the total cost of care and health needs of a population in a defined target region. Driving accountability to a local level empowers communities to devise strategies best designed to meet their health care needs, according to CMS.
Twenty-six regions for new program
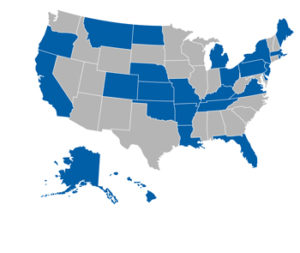 Primary Care First model options will be offered in 26 regions for a 2020 start date: Alaska (statewide), Arkansas (statewide), California (statewide), Colorado (statewide), Delaware (statewide), Florida (statewide), Greater Buffalo region (New York), Greater Kansas City region (Kansas and Missouri), Greater Philadelphia region (Pennsylvania), Hawaii (statewide), Louisiana (statewide), Maine (statewide), Massachusetts (statewide), Michigan (statewide), Montana (statewide), Nebraska (statewide), New Hampshire (statewide), New Jersey (statewide), North Dakota (statewide), North Hudson-Capital region (New York), Ohio and Northern Kentucky region (statewide in Ohio and partial state in Kentucky), Oklahoma (statewide), Oregon (statewide), Rhode Island (statewide), Tennessee (statewide), and Virginia (statewide).
Primary Care First model options will be offered in 26 regions for a 2020 start date: Alaska (statewide), Arkansas (statewide), California (statewide), Colorado (statewide), Delaware (statewide), Florida (statewide), Greater Buffalo region (New York), Greater Kansas City region (Kansas and Missouri), Greater Philadelphia region (Pennsylvania), Hawaii (statewide), Louisiana (statewide), Maine (statewide), Massachusetts (statewide), Michigan (statewide), Montana (statewide), Nebraska (statewide), New Hampshire (statewide), New Jersey (statewide), North Dakota (statewide), North Hudson-Capital region (New York), Ohio and Northern Kentucky region (statewide in Ohio and partial state in Kentucky), Oklahoma (statewide), Oregon (statewide), Rhode Island (statewide), Tennessee (statewide), and Virginia (statewide).
