Now is a good time for medicine and public health to put their acts together
January 2022 – The Journal of Healthcare Contracting

Prior to COVID-19, did you know the names of the medical officers of your state or county public health departments? Did the physicians you call on know their names?
It was the lack of coordination between medical providers and public health that led to failures in testing and vaccination during the pandemic, writes healthcare expert Atul Gawande in an August 2021 New Yorker article, “Costa Ricans Live Longer Than We Do. What’s the Secret?” In many cases, public health departments “were forced to launch their own operations, such as drive-through testing sites and stadium vaccination clinics – and they had to do so from scratch, in a mad rush.” More proof, he says, that the U.S. healthcare system “is designed for the great breakthrough – not the great follow-through.”
And it’s been that way for a long time.
Separate ways
From the start of the 20th century, public health and medicine developed as separate disciplines, notes the American Public Health Association (APHA). Medical and public health practitioners were educated in separate schools and upon graduation, the two disciplines went their separate ways.
But with escalating healthcare costs, continuing growth in the ranks of the uninsured, increasing emphasis on healthcare quality and outcomes, chronic disease, ever-widening health disparities, and outbreaks of emerging infectious diseases, greater collaboration between the two professions is not an option, but a pressing mandate, concluded researchers from the Florida State University College of Medicine in a study 15 years ago.
That’s just as true – or more so – today.
A matter of perspective
Here’s the problem: The two disciplines – medicine and public health – look at health very differently. In 1996, Donna Shalala, Secretary of Health and Human Services under President Clinton, compared them to trains on parallel tracks, with windows facing opposite directions. Those on the medical train see individual trees, with subtle differences in size, color, age and health, she said. Those aboard the public health train see a forest, that is, populations of similar trees, growing together and weathering the same storms.
Put another way, public health agencies define “population” on the basis of residential location, divided up by demographic factors such as race, ethnicity, gender, age, language, disability, or disease status, explains the American Academy of Family Physicians (AAFP) in its 2015 position paper on “Integration of Primary Care and Public Health.” Meanwhile, the medical community defines “population” as those individuals to whom a healthcare entity provides care – in other words, the practice panel. (And payers look at “population” in terms of the members of their insurance plans.)
What kind of a world would it be?
If a primary care practice were to become more integrated with the local public health department, physicians would consider more carefully the social and physical environments in which their patients live, and then work to improve health outcomes, says AAFP.
It might also lead to advocacy – even community activism – on the part of doctors.
“There is a growing and exciting understanding that much of what determines health happens outside the exam room,” Mark Del Monte, J.D., CEO of the American Academy of Pediatrics (AAP), told The Journal of Healthcare Contracting. “Medicine can play an incredibly important role collaborating with public health, community-based organizations, schools and local governments and working on the social drivers that are powering health disparities.”
In its Advocacy Guide, the AAP defines advocacy as “taking the care, the information, and the resources that you provide to individual children and families and sharing those stories and experiences at the community, state, or federal level to help create systemic change. Community advocacy takes into consideration the environmental and social factors influencing child health, such as exposure to violence, safe places to play, poverty, child abuse, and access to healthy foods, and addresses ways in which child advocates – including pediatricians – can work with community partners to address these issues.”
A data-driven approach
Advances in information technology, including medical records systems and geographic information systems (GIS), make collaboration between medical and public health professionals more feasible than ever.
Researchers from RAND Corp. point out that mapping hospitalizations for ambulatory-care-sensitive admissions, such as asthma or cellulitis, can identify small geographic areas in which community-level intervention may be needed. Health insurers can play a role too. The National Health Plan Collaborative, a group of health insurers aiming to reduce disparities in care, says that by geocoding the addresses of health plan enrollees and linking them to quality-of-care data, plans can identify “hot spots” of poor quality.
The RAND researchers found that one insurance carrier determined that Hispanic members with diabetes were less likely to receive LDL testing. Initially, they contemplated sending a mass, Spanish-language mailing to all Hispanic members with diabetes, reminding them of the importance of lipid testing. But using GIS, the plan mapped the distribution of members with diabetes in a predominantly Hispanic region, then focused on a small hot spot with many members who had not received LDL testing. They found that the neighborhood was linguistically isolated and as a result, they decided to focus their resources on a language-appropriate intervention in that area.
In October 2021, the Primary Care Collaborative, a nonprofit organization working to advance primary care, and the Robert Graham Center, a family medicine and primary care research organization, released a report, “Primary Care and COVID-19: It’s Complicated – Leveraging Primary Care, Public Health and Social Assets.”
“A key innovation of this report for both public health and primary care is this notion of the community health index,” says Del Monte, who in addition to his duties at AAP is vice chair of the Primary Care Collaborative, “They used a data-driven analytical process to describe the interrelatedness between primary care and public health. It’s very clear that if we don’t have a strong primary care system and a strong public health system, we fail to optimize either one of them.”
‘Wrong pockets’
Tradition and history aside, money – or the lack thereof – is one of the biggest factors preventing medical and public health professionals from collaborating.
“Public health and primary care both try to prevent illness and even address the upstream conditions – the social determinants of health – that cause poor health, but there is not enough funding for this type of integrated approach,” Seiji Hayashi, MD, MPH, FAAFP, chief transformation officer and medical director for Mary’s Center, a federally qualified health center in Washington, D.C., told The Journal of Healthcare Contracting.
Commenting on the PCC/Graham Center report, Hayashi points to siloed funding as one of the biggest barriers. “Stuart Butler from the Brookings Institution and other policy researchers have been writing about the ‘wrong pockets’ problem, where even though funding for housing, transportation, and education can improve health, there isn’t an appetite for healthcare to transfer money to other sectors,” he says. “Investing in primary care and public health that tries to prevent illness is counter to most parts of the healthcare industry, where more care means more money.”
“Funding is unfortunately a large barrier and often holds back progress,” says Julie Wood, M.D., MPH, AAFP’s senior vice president for research, science and health of the public. “Public health and primary care are both underfunded by disparate … systems that often have common interests but are not structured to work well together.”
Financially, public health has been particularly hard hit for the past 10 years or so. Since 2010, spending for state public health departments has dropped by 16% per capita and spending for local health departments has fallen by 18%, according to a KHN and Associated Press analysis of government spending. At least 38,000 state and local public health jobs have disappeared since the 2008 recession, and more than three-quarters of Americans live in states that spend less than $100 per person annually on public health.
In California, “public health nurses, microbiologists, epidemiologists, health officers and other staff members … are abandoning the field,” according to the analysts. “It’s a problem that temporary boosts in funding can’t fix.”
Bright spots
No one said it would be easy to integrate medicine and public health. But there are bright spots.
“It’s not a moment in time; it’s a transition,” says Wood. “There are exemplary practices and communities, but the most exciting progress we are seeing is a transition in training. Family medicine residents are training from this perspective now, longitudinally, throughout their residency – looking at the data of their community and applying it to how they practice both at the community and individual practice level. They are coming out of training already prepared with knowledge and skills of how to work with their public health colleagues and with community information.”
Says Hayashi, “The unprecedented expansion of community health centers through the Affordable Care Act and subsequent federal support increased primary care capacity in underserved communities. Many public health departments leveraged these new primary care access points to tackle public health crises. For example, public health and primary care have been working together to address the opioid epidemic. Reducing environmental hazards like lead poisoning is a public health/primary care success story with screening and remediation. We still have much to do, though.”
There are bright spots around the world from which U.S. medical and public health practitioners can learn. “The concept used in the U.S., however, comes from principles of Community-Oriented Primary Care (COPC), which was developed in rural South Africa,” says Hayashi. “Community health centers in the U.S. were founded on this principle, and they are accustomed to the idea of serving a geographically defined area. In fact, this is one of the grant criteria for health centers receiving money from HRSA, the federal agency that funds and oversees community health centers.”
In his New Yorker article, Gawande speaks about the Costa Rican healthcare system, which, he says, “braids together public health and individual health.” In that Central American country, the “ATAP” is a clinician who has the skills of a medical worker and a public health aide. A local primary care team called an “EBAIS,” consisting of a physician, nurse and ATAP, are assigned to groups of several thousand people, and call on them regularly at their homes.
Lessons from the pandemic
Experts believe that the time to integrate medical and public health is now, while the lessons of the pandemic are still fresh.
One in 500 Americans has died from the virus, and the U.S. COVID-19 death toll accounts for nearly 20% of the world’s deaths, despite the U.S. being just over 4% of the world’s population, point out the authors of the PCC/Graham Center report. This even though the U.S. had one of the earliest and most robust supply of vaccines.
“It does not matter that vaccines are developed if communities cannot access them or individuals do not want them,” the authors write. “This is where public health and primary care integration can help.”
But amidst the failures during the pandemic lay glimmers of progress.
In communities with the most robust primary care, the strongest public health infrastructures, and the fewest social vulnerabilities, residents were 42% less likely to die from COVID-19 and 12% less likely to get infected with the virus, as compared to communities on the other end of the spectrum, according to the PCC/Graham Center report.
The COVID-19 pandemic showed how primary care and public health together can save lives, says Hayashi. “Public health provided expertise, resources, and supplies like test kits and vaccines. Primary care was the vehicle to deliver the testing and vaccines. Hospitals played a large role, but primary care was the trusted source of information and care to keep people from needing to go to ERs and hospitals. I can’t call most of this a model of public health-primary care integration, but it’s a start.”
“There is opportunity for improvement in infrastructure across the country as we begin to consider recovery,” says Wood. “We are certainly thinking about the important role of primary care and especially collaboration with our public health colleagues and how we rebuild that partnership to be stronger together.”
“With a new shared understanding of the definition of population, the integration of primary care and public health can foster an effective collaboration that understands that the health of a population is not simply a product of functionality or funding of healthcare services,” says the AAFP in its position paper. “Rather, it includes the conditions in which people are born, grow, live, work, and age, and encompasses inequities in power, money, and resources.”
Says Wood, “Ideally, a practice is already a team, but when integrated with public health, the team is even bigger, with more resources and services to offer patients and the community. There’s also the opportunity to have more information, show outcomes and often seek funding to support these programs.” Some state AAFP chapters already work with their local or state public health departments to help with tobacco prevention and cessation programs and other wellness programs.
“Incremental changes make a difference as well. Partnering with community health workers or the public health department can broaden the reach beyond the walls of the clinic and be helpful to patients, the primary care physician, and their team.”
Pediatricians in the community
Since 1993, the Community Access to Child Health (CATCH) program of the American Academy of Pediatricians has given grants to support pediatric residents and pediatricians in planning or implementing community-based child health initiatives. According to AAP, potential roles that pediatricians can play at the community advocacy level include:
- Initiating a community project or forming a partnership, alliance, or coalition to address a problem.
- Informing community leaders, about issues affecting children in the community.
- Inviting decision-makers to visit their professional setting.
- Providing testimony and telling their story at community forums, events, and in the local media.
- Serving on the board of organizations that support children’s health well-being or interests, such as a school board.
- Offering medical expertise to schools, youth organizations or institutions, and child care centers.
Two perspectives
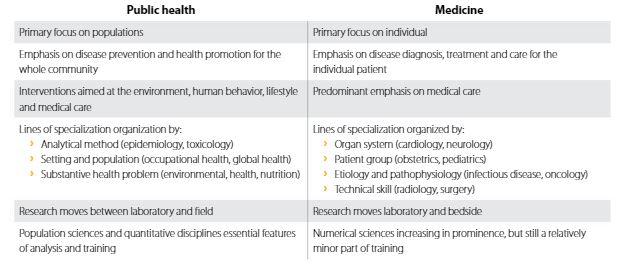
Editor’s note: This table, from the Harvard School of Public Health, demonstrates how differently medicine and public health view healthcare