HbA1c testing could play big role as Medicare addresses prediabetes
 Diabetes is at epidemic levels in the Medicare population, affecting more than 25 percent of Americans aged 65 or older, reports the Center for Medicare and Medicaid Services (CMS). Care for Americans aged 65 and older with diabetes accounts for roughly $104 billion annually, and these costs are growing. By 2050, diabetes prevalence is projected to increase two- to threefold if current trends continue.
Diabetes is at epidemic levels in the Medicare population, affecting more than 25 percent of Americans aged 65 or older, reports the Center for Medicare and Medicaid Services (CMS). Care for Americans aged 65 and older with diabetes accounts for roughly $104 billion annually, and these costs are growing. By 2050, diabetes prevalence is projected to increase two- to threefold if current trends continue.
Type 2 diabetes is typically preventable with appropriate lifestyle changes. That’s why, in March 2016, the Department of Health and Human Services announced its intention to launch a program in January 2018 that would reimburse providers for providing diabetes-prevention services to people at risk of developing Type 2 diabetes. The program, called the Medicare Diabetes Prevention Program (MDPP), would be modeled after a diabetes program developed by the Centers for Disease Control and Prevention.
In July, CMS issued proposed rules for the new program, including eligibility. Public comment was allowed until September 6.
What is prediabetes?
CMS defines a diabetes prevention program as an evidence-based intervention targeted to individuals with prediabetes, meaning those who have blood sugar that is higher than normal but not yet in the diabetes range. The risk of progression to Type 2 diabetes in an individual with prediabetes is around 5 to 10 percent per year, or about five to 20 times higher than in individuals with normal blood glucose, according to CMS.
As proposed by CMS, the Medicare program would mimic the CDC-administered program. That program – described as a structured health behavior change program – is delivered in community and healthcare settings by trained community health workers or health professionals. It consists of 16 intensive “core” sessions of a CDC-approved curriculum in a group-based setting, which provide practical training in long-term dietary change, increased physical activity, and problem-solving strategies for overcoming challenges to sustaining weight loss and a healthy lifestyle. After the 16 core sessions, monthly maintenance sessions help to ensure that the participants maintain healthy behaviors. The primary goal of the intervention is to reduce incidence of Type 2 diabetes by achieving at least 5 percent average weight loss among participants.
Who’s eligible?
CMS has proposed that coverage of Medicare Diabetes Prevention Program services be available for beneficiaries who meet the following criteria:
- Are enrolled in Medicare Part B.
- Have as of the date of attendance at the first Core Session a body mass index (BMI) of at least 25 if not self-identified as Asian, and a BMI of at least 23 if self-identified as Asian. (The CDC standards have defined a lower BMI for Asian individuals based on data that show Asians develop abnormal glucose levels at a lower BMI.)
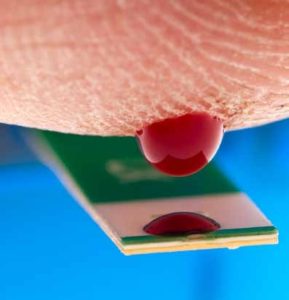
- Have within the 12 months prior to attending the first Core Session a hemoglobin A1c test with a value between 5.7 and 6.4 percent, or a fasting plasma glucose of 110-125 mg/dL, or a two-hour post-glucose challenge of 140-199 mg/dL (oral glucose tolerance test). (CMS uses this definition of prediabetes instead of the definition in the 2016 American Diabetes Association Standards of Care because the ADA standards includes the use of a hemoglobin A1c test to diagnose prediabetes and the CMS actuarial certification uses the World Health Organization definition of prediabetes as a fasting plasma glucose of 110-125 mg/dL.)
- Have no previous diagnosis of Type 1 or Type 2 diabetes. A beneficiary with previous diagnosis of gestational diabetes is eligible for the program.
- Does not have end-stage renal disease (ESRD).
Under the proposed rules, beneficiaries who meet the coverage criteria would be able to enroll in the MDPP only once. However, those beneficiaries who complete the 12-month program and achieve and maintain a required minimum level of weight loss would be eligible for additional monthly maintenance sessions for as long as the weight loss is maintained.
Who can provide services?
As of 2015, more than 800 organizations had preliminary or full recognition from the CDC Diabetes Prevention Recognition Program (DPRP) to provide DPP services. These organizations had served more than 40,000 participants. More than 60 health plans provide some coverage of DPP services.
In its July proposed rule, CMS proposes that any organization recognized by the CDC to provide DPP services – that is, those with preliminary or full recognition – be eligible to apply for enrollment in Medicare as a supplier beginning on or after Jan. 1, 2017.
Organizations seeking to enroll in Medicare specifically to become MDPP suppliers would be subject to screening under the “high categorical risk category” defined by existing Medicare provisions. CMS made that proposal in the belief that MDPP suppliers would probably bear some similarities to home health agencies, because non-medical personnel may deliver MDPP services in a non-clinical setting.
Editor’s note: To learn more about the National DPP please visit http://www.cdc.gov/diabetes/prevention/lifestyle-program/index.html.
For more information on the CDC-approved curriculum, which could be carried into the national Medicare program, go to http://www.cdc.gov/diabetes/prevention/pdf/curriculum_toc.pdf.
Prediabetes curriculum
The proposed Medicare Diabetes Prevention Program would use the diabetes-prevention curriculum approved by the Centers for Disease Control and Prevention.
During the first six months (weeks 1-26) of the intervention, each of the 16 core sessions must address one of these curriculum topics, and all topics must be addressed by the end of the 16 sessions:
- Welcome to the National Diabetes Prevention Program
- Self-Monitoring Weight and Food Intake
- Eating Less
- Healthy Eating
- Introduction to Physical Activity (Move Those Muscles)
- Overcoming Barriers to Physical Activity (Being Active – A Way of Life)
- Balancing Calorie Intake and Output
- Environmental Cues to Eating and Physical Activity
- Problem-solving
- Strategies for Healthy Eating Out
- Reversing Negative Thoughts
- Dealing with Slips in Lifestyle Change
- Mixing Up Your Physical Activity: Aerobic Fitness
- Social Cues
- Managing Stress
- Staying Motivated, Program Wrap-up
The last six months (weeks 27-52) of the DPP 12-month intervention must include at least one core maintenance session delivered in each of the six months (for a minimum of six sessions), and all core maintenance sessions must address different topics:
- Welcome to the Second Phase of the Program
- Healthy Eating: Taking It One Meal at a Time
- Making Active Choices
- Balance Your Thoughts for Long-Term Maintenance
- Healthy Eating With Variety and Balance
- Handling Holidays, Vacations, and Special Events
- More Volume, Fewer Calories (Adding Water Vegetables and Fiber)
- Dietary Fats
- Stress and Time Management
- Healthy Cooking: Tips for Food Preparation and Recipe Modification
- Physical Activity Barriers
- Preventing Relapse
- Heart Health
- Life With Type 2 Diabetes
- Looking Back and Looking Forward
What about reimbursement?
Providers would be reimbursed for services provided through the Medicare Diabetes Prevention Program at the times and in the amounts set forth below, with payment tied to number of sessions attended and achievement of a minimum weight loss of 5 percent of baseline weight (body weight recorded during the beneficiary’s first core session). MDPP providers would be required to attest to beneficiary session attendance and weight loss at the time claims are submitted to Medicare for payment. Each beneficiary’s attendance must be documented through paper or electronic means, and each beneficiary’s weight must be measured and recorded every MDPP session the beneficiary attends.
DPP Payment Model
| Payment per beneficiary (non-cumulative) | |
| Core Sessions | |
| 1 session attended | $25 |
| 4 sessions attended | 50 |
| 9 sessions attended | 100 |
| Achievement of minimum weight loss of 5% from baseline weight | 160 |
| Achievement of advanced weight loss of 9% from baseline weight | 25 |
| Maximum Total for Core sessions | 360 |
| Maintenance Sessions (Maximum of 6 monthly sessions over 6 months in Year 1) | |
| 3 Maintenance sessions attended (with maintenance of minimum required weight loss from baseline) | 45 |
| 6 Maintenance sessions attended (with maintenance of minimum required weight loss from baseline) | 45 |
| Maximum Total for Maintenance sessions | 90 |
| Maximum Total for first year | 450 |
| Maintenance Sessions After Year 1 (Minimum of 3 sessions attended per quarter/no maximum) | |
| 3 Maintenance sessions attended plus maintenance of minimum required weight loss from baseline | 45 |
| 6 Maintenance sessions attended plus maintenance of minimum required weight loss from baseline | 45 |
| 9 Maintenance sessions attended plus maintenance of minimum required weight loss from baseline | 45 |
| 12 Maintenance sessions attended plus maintenance of minimum required weight loss from baseline | 45 |
| Maximum Total After First Year | 180 |
—————————————————————-
HEAD: Pilot program at the YMCA
In 2012, the Center for Medicare & Medicaid Innovation (the Innovation Center) awarded a Health Care Innovation Award (HCIA) to YMCA of the USA (Y-USA) to test whether Diabetes Prevention Program services could be successfully furnished by non-physician, community-based organizations to Medicare beneficiaries diagnosed with prediabetes and therefore at high risk for development of Type 2 diabetes.
Between February 2013 and June 2015, the Y-USA, in partnership with 17 local YMCAs, the Diabetes Prevention and Control Alliance, and seven other non-profit organizations, enrolled a total of 7,804 Medicare beneficiaries into the model. Enrolled beneficiaries represented a diverse geography across the eight states of Arizona, Delaware, Florida, Indiana, Minnesota, New York, Ohio, and Texas.
Medicare beneficiaries demonstrated high rates of participation and sustained engagement in the program. Approximately 83 percent of recruited Medicare beneficiaries attended at least four core sessions, and approximately 63 percent completed nine or more core sessions.
Weight loss is a key indicator of success among persons enrolled in a DPP, according to CMS. Those beneficiaries who attended at least one core session lost an average of 7.6 pounds, while beneficiaries who attended at least four core sessions lost an average of 9 pounds. BMI was reduced from 32.9 to 31.5 among Medicare beneficiaries who attended at least four core sessions.
Independent evaluation reports are available on the Innovation Center’s website at https://innovation.cms.gov/initiatives/Health-Care-Innovation-Awards/
