Long-term stockpiles present an unworkable mix of management, logistical, and financial challenges for healthcare providers
By Linda Rouse O’Neill, HIDA VP of Government Affairs
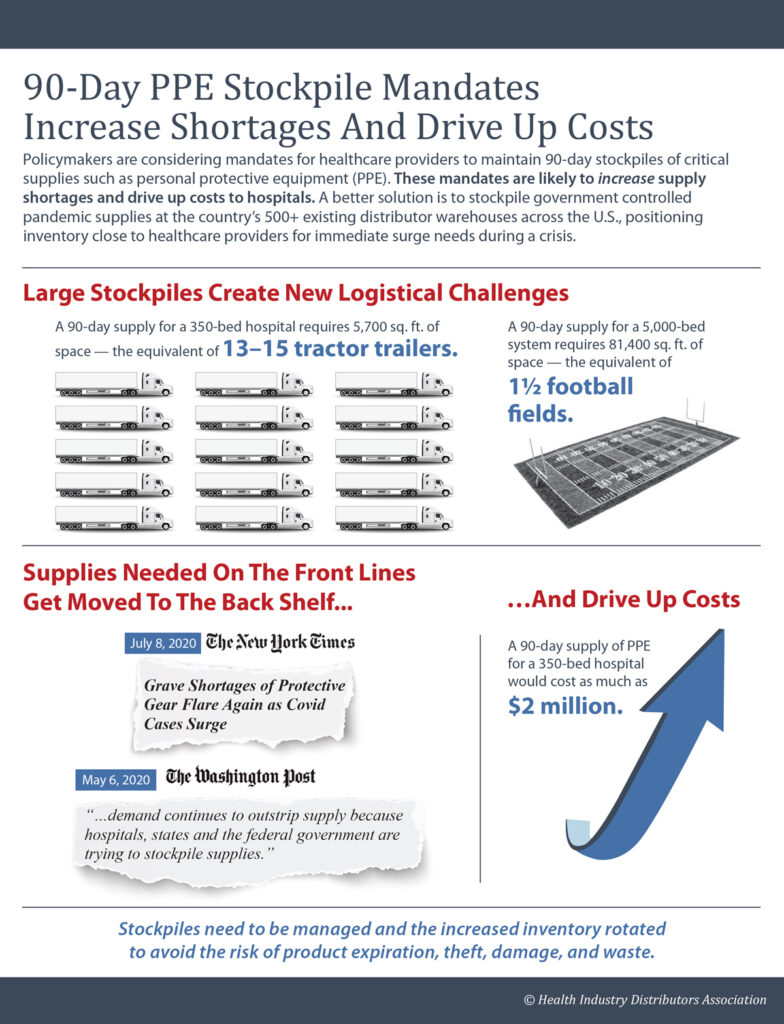
Proposals requiring healthcare providers to maintain a 90-day stockpile of personal protective equipment (PPE) and other critical supplies appear to be a simple way to avoid future equipment shortages. In reality, requiring every hospital and nursing home to maintain a sizable stockpile in the middle of global pandemic will exacerbate ongoing PPE shortages. Stockpiles of this size divert supplies from the front lines to the back shelf of a warehouse.
HIDA and fellow trade association AdvaMed wrote to New York’s Health Department and Governor’s Office to share concerns about the state’s 90-day mandate. Together, we urged the state to utilize the private sector’s innovation and experience with manufacturing, storage, warehousing and technology to help ensure New York’s public health goals.
“Leveraging experienced supply chain experts will avoid the risk of product expiration, theft, damage, and waste,” we wrote in the letter. “Further, we are concerned that hospitals in New York will not be able to meet the logistical challenge of this stockpiling requirement. A 90-day supply for a 350-bed hospital requires 5,700 square feet of space, which is the equivalent of approximately 15 tractor trailers.”
Efforts to create larger equipment reserves are one reason why demand continues to outstrip supply. Imposing a 90-day stockpile mandate on every hospital would create even greater shortages. Stockpiling incurs additional costs and complications happening when hospitals are reeling from the impact of the pandemic. Many are suffering a steep decline in revenue due to canceled or postponed elective surgeries that can generate up to 50% of a hospital’s operating revenue.
A better approach is to leverage the proven expertise of health industry distributors. Distributors have the infrastructure ready to provide storage, logistics support and the expertise to manage the range of costs, operational, and logistics issues. All this can be done while building a new national pandemic response infrastructure capable of replenishing supplies.
One component of that infrastructure would be forward-deployed reserves of supplies to meet the first-call needs of healthcare providers when a crisis strikes. Based at the 500 commercial distribution centers across the country or government warehouse, the federal government would manage and control the stockpiles. Distributors would manage them to ensure the inventory is rotated and replenished.
In addition to reserves, the pandemic response infrastructure would include expanded, diversified surge manufacturing capacity with a strong focus on domestic production and centralized federal stockpiles to meet the emergency needs of state and local governments. Relying on forward-deployed reserves would relieve providers of the expense and administrative burdens of maintaining massive stockpiles of their own and enable hospitals to keep doing what they do best: care for patients.
Lawmakers are considering language originally introduced in the Medical Supplies for Pandemics Act of 2020 that would implement this framework. It would authorize funds to implement a supply chain flexibility manufacturing program creating incentives for U.S. manufacturers to improve supply chain elasticity.