SPONSORED: MCKESSON
How an experienced strategic partner can help health systems create – and navigate – an effective non-acute strategy
 Changes in virtually every facet of the healthcare industry – including legislation, health insurance, technology, and clinical innovation – continue to create new challenges for healthcare systems to navigate. No one is feeling the impact more than that of supply chain leadership, whose responsibilities now include everything from surgery centers and physician’s offices to nursing homes and the patient’s home.
Changes in virtually every facet of the healthcare industry – including legislation, health insurance, technology, and clinical innovation – continue to create new challenges for healthcare systems to navigate. No one is feeling the impact more than that of supply chain leadership, whose responsibilities now include everything from surgery centers and physician’s offices to nursing homes and the patient’s home.
Managing the non-acute continuum can be particularly challenging due to the complexity and fragmentation across so many care settings. Quite often you are dealing with locations that are geographically dispersed, have different care requirements, and operate separately from one another, even acting like micro-supply chains. The non-acute supply chain may represent a small portion of total spend, but can have many more people placing orders, adding complexity.
Each health system faces new, evolving challenges in streamlining the way they manage and coordinate logistics for their non-acute continuum. Challenges abound within supply chain management, handling multiple clinical infrastructures across different specialties, with various value-based-care driven financial models.
To get the most out of your health system’s investments in the care continuum, supply chain leaders need a comprehensive strategy to address the many facets of non-acute. The Journal of Healthcare Contracting has worked with McKesson Medical-Surgical, a leader in non-acute care supply chain strategies, to develop a roadmap for driving out costs and providing better care.
The Roadmap to Success in Health Systems for Non-Acute Continuum
 The acute care supply chain involves a team of people trained to handle the influx of products, breakdown of pallets and putaway in the hospital. It is a carefully synchronized production. As health systems acquire alternative care sites, these care sites have their own supply chain requirements, separate technology, and ways of handling their supply chain. It becomes more difficult for operations leadership to manage a fragmented and complex non-acute supply chain. There can also be more risks involved:
The acute care supply chain involves a team of people trained to handle the influx of products, breakdown of pallets and putaway in the hospital. It is a carefully synchronized production. As health systems acquire alternative care sites, these care sites have their own supply chain requirements, separate technology, and ways of handling their supply chain. It becomes more difficult for operations leadership to manage a fragmented and complex non-acute supply chain. There can also be more risks involved:
- Delivery challenges with few or non-existent loading docks, more putaway locations
- Not meeting regulatory requirements; clinical quality might be impacted
- Multiple purchase orders and invoices per site
- High carrying costs, more inventory and product expiration costs associated with more inventory
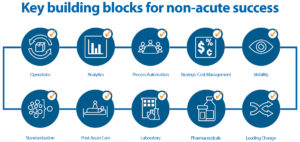
To deliver better outcomes for their patients, health systems should maximize the performance of their non-acute settings with a multi-pronged approach incorporating ten key areas of optimization. This will allow health systems to:
- Take control of their supply chain and financial performance
- Improve their clinical infrastructure as required by today’s patients and current reimbursement models
- Take the next step to deliver the highest quality of patient care possible
- Lead organizational change to execute initiatives and achieve goals
1. Operations: Operational Expenses and Productivity
How many different vendors are providing supplies across your non-acute care settings? The more suppliers involved in your ambulatory and post-acute supply chain, the more likely you are missing cost savings opportunities, losing valuable staff time, and providing inconsistent quality of care. There is more time and labor involved in handling multiple deliveries. There are varying price structures across the non-acute sites. There can be incorrect tier rostering and more.
The single most important consideration is to make sure your operational model is designed to meet the specific needs of each of the individual care settings. In the non-acute settings, it’s not a one-size-fits-all model. From the delivery model to the enabling technologies, supply chain has to evaluate and make critical decisions on which solution helps to drive down operational expenses while improving staff productivity. It’s extremely important that clinic staff spend their time on patient care and not on PAR levels.
2. Analytics: Visibility and Insights
Without proper technology and expertise, it’s nearly impossible to gather accurate, comprehensive data across all non-acute sites within a system. It’s important to have a tool that can bridge the data gaps within your health system. It’s not uncommon for non-acute sites to have different technology than the hospitals, and even different technology from each other. A supply chain solutions partner should bridge the gap to provide the breadth of visibility that goes beyond the operations within one’s own facility to help consultatively provide insights on additional cost-saving measures and process improvements to enact across the health system.
What are the ordering trends across your non-acute settings? Do you know the rate of usage of your most frequently ordered supplies? Having this data readily accessible can enable you to predict and automate future orders so that clinicians can focus on patient care instead of on product inventory.
What are similar facilities and clinicians ordering? Insight and access to peer analytics can be invaluable for supply chain decision support and standardization. Standardizing leads to optimum quality of care and efficiency. Having this data at your finger tips can enable better decision making.
3. Process Automation: Productivity, Accuracy and Speed of Business
How automated are your current non-acute supply chain processes? Automation is paramount to keeping costs down, and the quality of care up, according to Liz Hayes, Health Systems Technology Manager at McKesson. “Connectivity across the non-acute supply chain is critical, including connectivity to EMR, EHR, and ERP systems,” she explains. “Any point that we can assist in automating a process to remove manual labor from that equation assists the health system in achieving their goals, including formulary compliance, increased efficiencies, and software integration.” If you can automate back-end office functions, like procurement, you give more time back to the clinicians to spend on patient care and improve provider satisfaction.
4. Strategic Cost Management: Contract Leverage
Do you have a strategy that drives your underlying product cost decisions? Is it based on GPO compliance or on the lowest cost? How are you leveraging your aggregated volume to negotiate vendor contracts? How are you operationalizing these cost source strategies?
Negotiating a great contract is just the beginning when it comes to driving down the cost of products. There are several areas to consider when tackling strategic cost management. First is access to the data necessary to make informed decisions. With the right data you can match product ordering to usage in order to standardize products across your non-acute settings. This can lead to greater leverage with suppliers when it comes to cost negotiations.
Many health systems focus on getting the lowest price for a given item, but there is so much more that factors into overall supply chain costs. For example, issues such as late, inaccurate or damaged deliveries and storage issues can impact clinical outcomes in addition to financial performance. As you consider the total cost of your operations, be sure to factor in these costs. Be careful with activity-based pricing models that are not aligned with your system needs. These may cost you more in the long run.
Finally, aligning stakeholders and agreeing on a project plan can be critical to the success of these programs. Having an experienced partner solely focused on non-acute can help you take advantage of cost sourcing opportunities.
5. Visibility: From Physician’s Office to the Patient’s Home
How does visibility into your system’s non-acute settings drive overall business goals?
“As care moves out of the acute setting and into specialized non-acute settings, it becomes even more critical to ensure supply chain financial and decision support in those care settings,” states Jacob Hookom, Vice President of Customer Experience, Information Technology at McKesson. “This visibility helps improve your bottom line, and can help identify and measure operational efficiencies, care standardization, and contract compliance outside the four walls of the facility.”
Hookom and his team help health systems manage data for their non-acute facilities to implement initiatives like product standardization. Implementing standardization and reducing clinical variation can help drive down costs and improve patient outcomes. “Product standardization leads to care standardization which impacts costs,” he explained. Having an integrated system that provides access and visibility to the right data can drive clinical decisions at both a macro level, across the health system, and at the micro level, within the individual specialty setting. It helps to contain costs and prevents discrepancies in patient care.
6. Standardization: Product and Processes
How does your system ensure that all non-acute locations are on formulary, and are meeting compliance goals?
Although non-acute settings vary, there is still room for standardization of supply chain processes. The process of standardizing non-acute supply chain operations begins with the quality and scope of the data and analytics available to those responsible for supply chain operations. A successful standardization effort can lead to better financial, clinical and operational performance. This leads to reduction in clinical variation. Standardization should happen across all product lines: medical/surgical, pharmaceutical, equipment, and lab. Utilizing non-acute specialists can help take some of the emotional decision-making out of the process.
How do clinicians know what is the best product, application, and utilization of supplies for each non-acute episode of care?
New technology, new products, and equipment are continuously entering the market. Often these new supplies require clinical training. With analytics and decision support, you can better train your clinical population to provide a more consistent level of care.
7. Post-Acute Care: Meeting Care Requirements Post-Discharge
How and where are medical supplies currently delivered to your organization’s post-acute care settings? If post-acute supplies are not being delivered directly to clinicians or patients at the point-of-care (including home health settings), clinicians may be wasting valuable time chasing down supplies, or patients may not have the necessary products to care for themselves properly at home.
Is your post-acute supply chain process designed for optimum efficiency, effectiveness, and quality of care to prevent patient readmissions? Patients who are released from a hospital to a post-acute facility, and then end up being readmitted due to an infection or post-surgical complications, can negatively impact a health system’s reimbursement. Twice: initially at the hospital, and again in the post-acute setting. 18 percent of patients discharged to a post-acute care facility are readmitted to the hospital within 30 days.* [https://www.ncbi.nlm.nih.gov/pubmed/27981557]
“Technology and product formulary management play a significant role with our post-acute care providers – it’s the key to reducing hidden costs,” said Deborah Haywood Vice President of Strategic Segments for Extended Care at McKesson. The Extended Care team helps providers develop a strong post-acute strategy that optimizes two key facets of care: distribution of the medical supplies to the point of care and proactive product formulary management.
8. Laboratory: Diagnosis and Convenience
How focused is your lab strategy on workflow efficiency as it relates to operational, clinical and financial feasibility? How integrated are your supply chain and lab functions – do they work together to impact revenue, increase patient satisfaction and clinical outcomes?
Lab represents two percent of healthcare spending and influences 70 percent of medical decisions*. [http://www.clpmag.com/2016/03/value-diagnostics/]
“Supply Chain often doesn’t understand that they can have a significant impact on lab,” said Lynn Glass, Vice President of Strategic Accounts for McKesson. “Set up properly, lab can generate revenue,” as opposed to being a cost center, according to Glass. Her team at McKesson offers strategies and solutions for laboratory supply chain professionals to implement in non-acute settings, including point-of-care testing, cutting-edge tools and technology, and comprehensive data and analytics. These cutting-edge solutions help laboratory clinicians and administrators integrate corporate supply chain and lab processes to achieve best practices such as standardization, SKU optimization, and supply chain utilization strategies that incorporate input from the biomedical board or clinical representative.
9. Pharmaceuticals: Availability and Regulatory
How does your health system ensure that non-acute clinicians are meeting formulary and regulatory requirements for ordering, managing, dispensing pharmaceuticals, as well as disposing of unused drugs? How many suppliers are involved in providing pharmaceuticals to non-acute sites?
The pharmaceutical supply chain is yet another area in which consolidation of suppliers and standardization leads to synergies across all settings. It can provide valuable cost savings, increase quality of care, improve patient experience, and streamline processes for optimum efficiencies.
How do your non-acute sites operate around backorders and varying availability (or unavailability) of products, without impacting patient care or financial outcomes?
Each non-acute setting needs the right drug available to complete each patient encounter appropriately. According to Patrick Baranek, Director, Pharmaceutical Sales at McKesson, a reputable distributor can help health systems achieve many efficiencies among their non-acute pharmaceutical supply needs. Having a pharmaceutical distribution strategy will help systems establish and manage a set formulary that considers all variables such as unit of measure, chain of custody, temperature requirements, and other regulatory requirements, such as USP800, and financial considerations. Having a pharmaceutical supply strategy is an important piece of the bigger non-acute strategy. By streamlining the way health systems manage pharmaceuticals in their non-acute continuum, they are better able to have a streamlined system with fewer invoices, fewer deliveries, and increased compliance in electronic ordering. This can help reduce administrative costs, and overhead, while maintaining the highest level of quality, safety, and patient care.
- Leading Change: Stakeholder Alignment and Initiative Execution
Healthcare is always changing. Effectively managing through these changes requires great alignment of stakeholders and processes. Do you speak the same language as your stakeholders? Do you understand their goals? Do they understand how you can help them achieve those goals?
One of your greatest challenges might be getting buy-in from the many stakeholders across the non-acute continuum. If so, you’re not alone.
Greg Colizzi, Vice President of Health Systems Marketing for McKesson, explains:
“For an organization to implement a comprehensive non-acute strategy, it requires the disciplines inherent to the supply chain – stakeholder alignment, process planning, analytics and project management. This evolution in healthcare represents a great opportunity for supply chain leaders to use their unique talents to take a broader leadership role across the health system.”
Colizzi’s team created this roadmap to improve operational performance. “Very few systems have the tools, resources and capabilities in-house to execute initiatives across the entire non-acute continuum effectively and efficiently.”
“Doing so requires expertise in the many facets of these individual care settings. We work closely with health systems to understand their unique challenges, assess processes, identify areas for improvement and help them lead change in their organization. We do this by deploying our specialized resources to execute on this roadmap, including operations, Six Sigma, laboratory, pharmaceuticals, process automation, post-acute care, analytics, standardization, and many more.” Colizzi added.
His team helps systems perform these assessments efficiently, objectively, and comprehensively allowing for more informed decisions. “We help systems overcome organizational inertia by providing a vision that all team members can rally around.” Colizzi explained.
Take control of your fragmented and complicated non-acute supply chain. Do any of these non-acute supply chain challenges sound familiar to you? This is where an experienced, strategic non-acute specialist can provide invaluable resources for health systems. We will explore opportunities for supply chain enhancement in upcoming articles featured in the weekly e-newsletter that will go in-depth into each of the ten key components of a strong non-acute supply chain. Each chapter will examine specific examples of how the roadmap will impact your health system’s operational, clinical, and financial performance and outcomes.
To learn more visit www.mckesson.com/takecontrol
